| Patient SafetyNet Home | Overview & Clinical Benefits | Enabling Technology | Halo Index | Resources |
Enabling Technology
Masimo SET® Pulse Oximetry
The accuracy and reliability of Masimo SET® significantly reduces false alarms and makes accurate clinician notification on the general floor possible
When identifying general floor monitoring solutions some hospitals look to scale their telemetry system to the general floor. However ECG telemetry is not optimal for monitoring non-cardiac post-surgical patients because:
|
Oxygenation monitoring, as recommended by both The Joint Commission and Anesthesia Patient Safety Foundation, provides an earlier indication of respiratory depression. Given nurse-to-patient ratios, patient ambulation, and rising patient acuity on the general floor, the chosen pulse oximetry technology must be able to measure through challenging conditions while minimizing false alarms. Masimo SET® is the best pulse oximetry choice for patient safety, clinical efficacy, and cost effectiveness.1 |
True and False Alarm Rates During Challenging Conditions
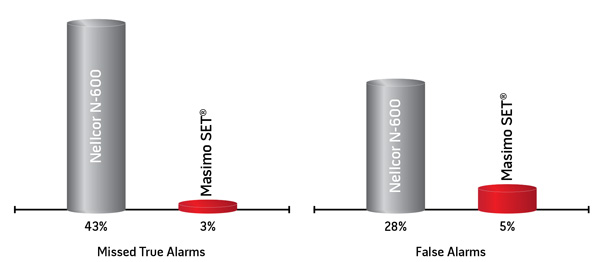
In this hospital-based study, investigators measured SpO2 in 10 subjects during motion and low perfusion conditions and calculated the false alarm rate during 120 full oxygenation events (specificity) and true alarm rate during 40 de-oxygenated events (sensitivity).2
Evidence-Based Alarm Management
| > | Earlier alarm notification without extending averaging times during challenging conditions like the Nellcor N-600 |
| > | Alarm reports enable evidence-based settings to titrate alarm frequency to acceptable levels for general floor clinicians |
| > | Configure alarm rules remotely or at the bedside to provide maximum clinical flexibility |
Value of Patient SafetyNet
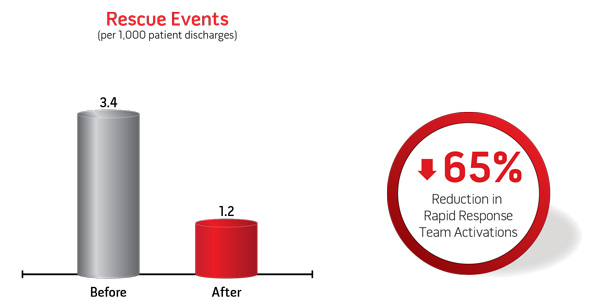
Proven to Help Improve Clinical Outcomes3
| Since Patient SafetyNet was instituted on a postsurigcal orthopedic unit at Dartmouth Hitchcock Medical Center in 2007, there have been no patients that have suffered irreversible severe brain damage or death as a result of respiratory depression from opioids. | In their initial 11 month evaluation of Patient SafetyNet on a single 36-bed orthopedic postsurgical unit, they demonstrated significant reductions in rapid response team activations and ICU transfers:3 |
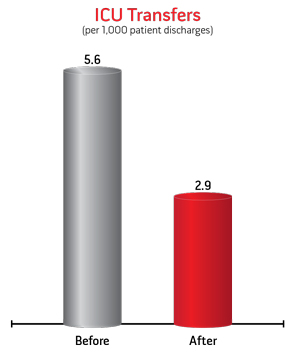
| > | Due to the decreased ICU transfer rate an annualized total of 135 days in the ICU were saved |
| > | Upon expansion of the system to all post-surgical units, a second unit realized a 30% decrease in ICU transfer rate and a corresponding annual total of 168 days in the ICU saved.4 |  |
|---|

"In my opinion as Quality and Safety Officer, our study results strongly demonstrate that continuous patient surveillance with Masimo SET® and Masimo Patient SafetyNet increases healthcare value by significantly improving clinical outcomes while reducing costs."
George T. Blike, M.D.
Medical Director, Patient Safety,
Dartmouth-Hitchcock Medical Center
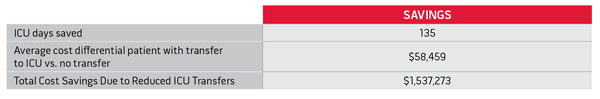
Proven Cost Effectiveness
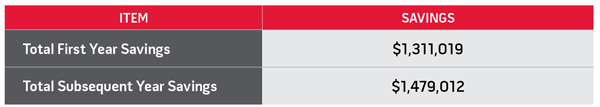
| When analyzing the financial impact of the reduction in ICU transfers and the reduction in ICU length of stay for a patient with transfer, versus the implementation and operating expenses associated with the system, the realized annual opportunity cost savings was $1.48 million on a single post-surgical unit. The cost per patient per hospital episode was just $22. | Cost-effectiveness was based on reduction of ICU transfers and days spent in the ICU. These costs are dependent on institutional factors and will vary from institution to institution. Capital and operating finance options are available. |
Hospital Opportunity Cost Savings on One Unit Due to Reduced ICU Transfers
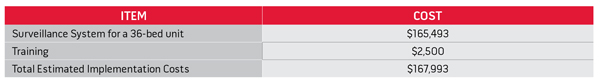
Estimated Implementation Costs
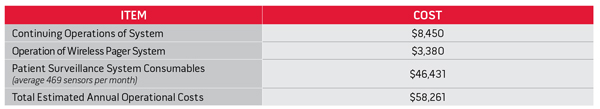
Estimated Annual Operational Costs
Total Savings
|
Patients with untreated moderate or severe obstructive sleep apnea (OSA) show increased risks of in-hospital complication, readmission, and developing various health conditions, and the economic costs of undiagnosed OSA patients can be as much as double that of non-OSA patients. The prevalence of OSA in the adult surgical population has been estimated to be as high as 22%, with 70% of those patients being undiagnosed.5 While screening efforts identify a portion of OSA patients, studies have shown that |
most of the screening tests will miss a significant proportion of patients with obstructive sleep apnea.6 The Patient SafetyNet system allows you to continually monitor patients’ oxygenation and respiration rate overnight. Reporting tools enable you to identify patients who may be experiencing oxygen desaturations and/or respiratory pauses, and who may benefit from further diagnostic evaluation. |
"The powerful reporting features of Patient SafetyNet have helped us identify patients that are at risk for sleep apnea and may benefit from a sleep study. Thus generating revenue for the hospital and helping to decrease healthcare system costs by identifying this critical risk factor earlier and enabling treatment of these patients."
Jon Carlson, Director, Respiratory Care Services |
|---|
Accurate and Patient-Tolerant Ventilation Monitoring
Respiration rate is a critical vital sign that provides early detection of respiratory compromise and patient distress
Oxygenation monitoring by continuous pulse oximetry is proven to improve clinical outcomes and reduce costs. However for patients receiving supplemental oxygen, pulse oximetry can be a late indicator of deterioration and thus ventilation monitoring is indicated.7 End tidal CO2 is capable of monitoring ventilation but it has been shown to have limitations in the spontaneous breathing patient. Patient tolerance, and potential removal of cannula and/or mask, is a notable limitation.8 Such a scenario may lead to alarms or even absence of patient monitoring.
The compelling need for a reliable respiration rate monitor to improve patient safety led Masimo to develop rainbow Acoustic Monitoring™ technology.
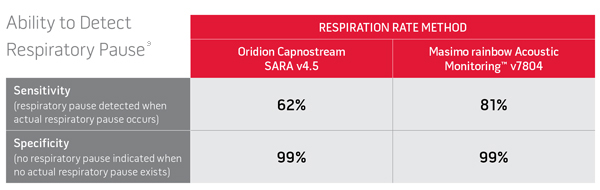
Retrospective analysis of 34 PACU subjects. Reference respiration rate determined by expert observer. A total of 21 episodes of respiratory pause were identified, defined as 30 seconds with no breathing activity.

| > | rainbow Acoustic Monitoring™ noninvasively and continuously measures respiration rate using an innovative adhesive sensor with an integrated acoustic transducer that is easily and comfortably applied to the patient’s neck. |
| > | End-tidal CO2 monitoring is also available on Patient SafetyNet. |
References
- Clinically proven in over 100 plus independent and objective studies.
- Shah N et al. J Clin Anesthesiology. 2012. 3 Blike G, MD. AAMI Medical Device Alarms Summit. October 2011.
- Taenzer AH et al. Anesthesiology. 2010;112(2):282-287.
- Taenzer AH et al. Anesthesia Patient Safety Foundation Newsletter. 2012.
- Finkel KJ, et al. Sleep Med. 2009;107:753-758.
- Ramachandran K, et al. Anesthesiology. 2009;110:928-39.
- Weinger MB, et al. APSF Newsletter. 2011:26(2):21-40. http://www.apsf.org/newsletters/pdf/fall_2011.pdf.
- Mimoz O, et al. British Journal of Anaesthesia. 2012;108(5):872-5.
- Ramsay M, et al. PGA. 2011;P9137. (abstract)